Egg donation is a fertility treatment that involves using donated eggs. This process is possible thanks to women who donate eggs altruistically. Egg donation is becoming increasingly common, and it achieves miracles for women who cannot achieve a pregnancy using their own eggs.

With IVI, you can access one of the world’s largest egg banks. This means it is easier to find the perfect donor match for you without the long waiting lists.

We aim to provide as much information as possible about your donor, so you can learn about them as a person. As well as their physical characteristics, you can also find out about their hobbies, interests, educational background and their motivation to donate eggs.

Using genetic compatibility testing, we can detect and avoid the possibility of passing down hereditary diseases to your baby.

We are pioneers in using artificial intelligence in our laboratories, which has allowed us to improve the process of embryo selection. By harnessing this technology, we can identify and prioritise the embryo most likely to achieve a pregnancy.

Your mental well-being as a future parent is important. You will have access to our highly qualified in-house fertility counsellors for support throughout your treatment.
Egg donation, sometimes called Donor Egg IVF, offers the possibility of achieving a pregnancy for patients who may not be able to do so with their own eggs. The treatment process is similar to a standard IVF (in vitro fertilisation) cycle, but instead, we mix sperm from the recipient couple with eggs provided by a donor. For single women opting for egg donation, donor sperm is used. We then transfer the resulting embryo to the womb of the female partner to achieve a pregnancy.


At IVI, we are committed to offering our patients the most effective treatment while ensuring the safety of mother and baby. That is why our success rates correspond to Live Birth Rate (LBR) per Embryo Transferred, in line with our Single Embryo Transfer (SET) policy.

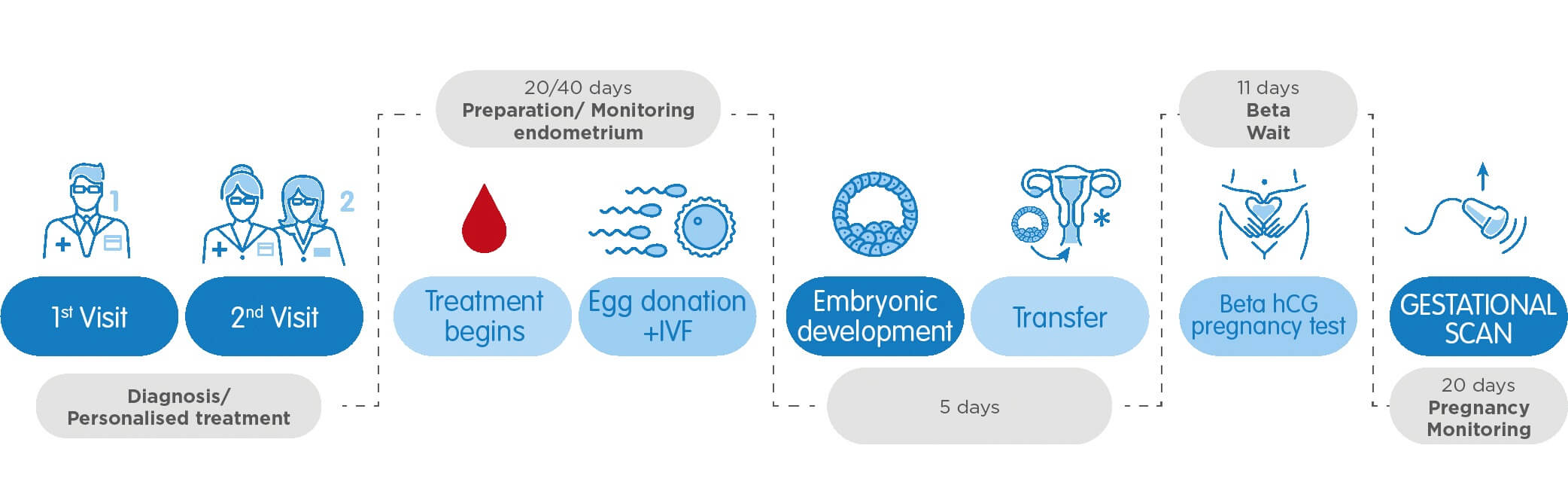
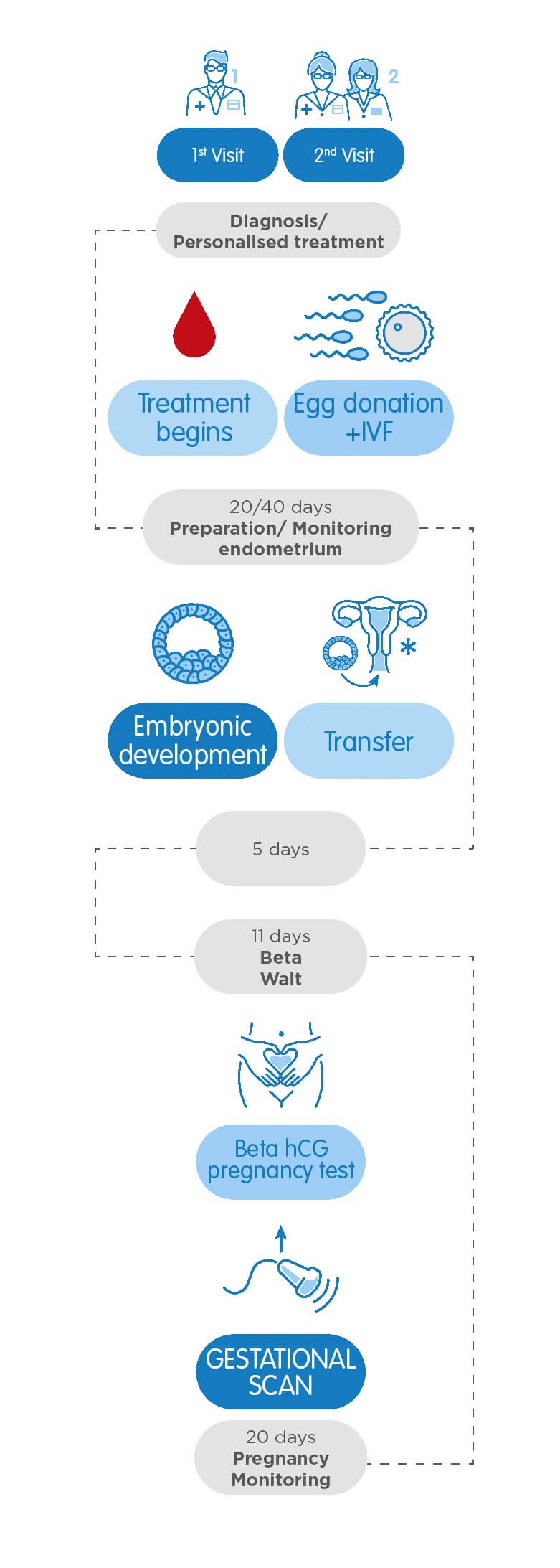

At your first appointment, your consultant will discuss your medical history and perform a pelvic ultrasound scan. Your results will also be reviewed if you’ve had fertility treatment in the past. If you’re part of a heterosexual couple, we will request a semen analysis if required. If your consultant recommends IVF with donated eggs, they will discuss the different treatment pathway options.

At your second appointment, you will meet with our Egg Donation Coordinator, who will explain the step-by-step process of your treatment. Afterwards, you will have a counselling session with one of our in-house counsellors, who will ensure you understand the implications and legal aspects of egg donation. We will carefully evaluate your potential donors, taking into account medical factors such as genetic compatibility and, if desired, physical characteristics such as complexion, height, eye colour and hair colour.

Once the donor eggs are ready, fertilisation will take place in the laboratory. At the same time, you will start taking medication to prepare your womb lining for embryo transfer. This lasts approximately 10 days and maximises the chances of an embryo successfully implanting. We will monitor your progression throughout this time using ultrasound scans and blood tests.

After selecting the highest quality embryo, our specialists will transfer the embryo to your uterus through a tiny cannula. This painless procedure is performed without anaesthesia. After resting for a few minutes, you can carry on your day as usual.

Approximately 11 days after the transfer, we will take a blood sample to perform a Beta-hCG test. This test measures the levels of pregnancy hormone (HCG) in your blood. If positive, we will perform an early pregnancy scan 20 days later. You will be discharged to begin your antenatal care if an ongoing pregnancy is confirmed.

The week-by-week progression of pregnancy, both in natural pregnancy and in assisted reproduction, is counted from the start date of the last period, with the probable due date being about 40 weeks later. If your last period was induced by hormonal medication, it is still counted as the start date and the weeks of pregnancy are counted from that date.
Another option is to take the embryo transfer date and add two weeks, which is approximately the time elapsed between the date of the last period and the fertilization of the oocyte and the first days of embryonic development.
In general, once you are matched with a donor, treatment can range from 1.5 – 2 months. It is important to remember that it is necessary to carry out all the medical tests, wait for the results, and compare them with those of the donor to ensure an appropriate match.
Egg donation treatments are high-performance procedures in which it is possible to achieve pregnancy in approximately 60% of cases. With 3 attempts, it is possible to reach cumulative pregnancy rates of 90%. Its performance does not depend on age, which is why it is considered an excellent alternative for all those women who have not managed to get pregnant with their own eggs.
It must be taken into account that the final cost may vary according to your unique requirements, such as pre-treatment tests and medication. These costs, which are charged separately from the package, will be provided after your initial consultation so you will know the final cost of your treatment before you decide to proceed.
This treatment is often recommended in cases of poor egg quality, such as for age-related reasons, or if you have had multiple unsuccessful IVF attempts with your own eggs.
Thanks to the research carried out at IVI on epigenetics, we know that the uterine environment greatly influences the development of the foetus. The dialogue between the uterine environment and the embryo during the months of pregnancy causes an important genetic exchange to exist, which may influence its future physical and psychological traits.


Located within a 10-minute walk from Oxford Circus, the IVI London clinic is a state-of-the-art facility offering a complete range of fertility treatments including IUI, IVF, ICSI and Egg Donation.